About.
Electrocorticography {ECoG} has been used for more than five decades to provide a wide array of vital information to the neurosurgical teams. ECoG being done for monitoring electrical cortical activity and mapping as well .
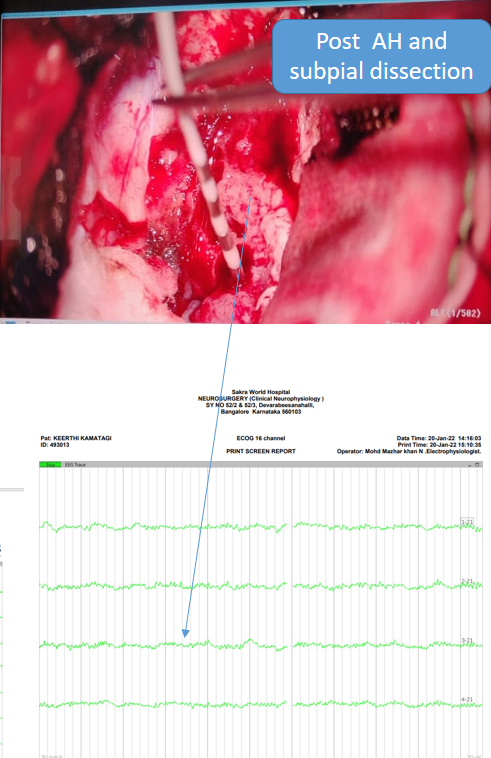
- It is commonly we use during the surgical treatment of epilepsy syndromes and is particularly useful for the localization or mapping of epileptogenic brain tissue, both the irritative zones and the epileptic foci. Electrocorticography also helps to determine the prognosis of the surgical outcome by analyzing any residual epileptiform activity { To eliminate the residual epileptogenic tissue or area, surgical and neurophysiological team usually preferer subpial dissection under 4-6 contact grid electrode to better outcome } this technique is currently being used by the majority of epilepsy centers all over the world.
History.
- Electrocorticography/Intraoperative electroencephalographic recordings were initially pioneered in human patients by Hans Berger [1929], who placed electrodes on the dural surface of patients with skull defects.
Picture of Professor Hans Berger.
- In the 1950s and 1960s, several investigators began using increasingly refined measures to study the local field potentials of various cortical locations as well as the pathological responses of epileptogenic tissues [Ajmone Marsan et al, 1958, Bancaud et al, 1965, Walker et al., 1961].
- In addition electrophysiologic responses to low intensity stimulation were found to be variable between cortical networks and were pathologically enhanced in epileptic tissue such that rhythmic spikes and waves were produced (Ajmone Marson, 1980; Ajmone Marsan et al., 1973; Bates, 1963; Bengzonet al., 1968; Gloor, 1975).
- In the recent era this electrophysiologic responses to low intensity stimulation also known as a Seizure onset localization zone[SOLZ].

Utility of Electrocorticography .
- Usually two type of recording being done during procedure .
- Direct recording from the cortex known as Electrocorticography.

- Another is Depth recording to confirm seizure onset zone like before amygdalohippocampectomy or other structure.
Localization of Seizure Onset.
- Electrocorticogram helps neurosurgeons precisely pinpoint the location where seizures originate in the brain. By placing electrodes directly on the surface of the brain (the cortex), ECoG records electrical activity with high spatial resolution. This information is essential for identifying the specific brain regions responsible for generating seizures.
Mapping of Functional Areas.
In addition to identifying seizure onset zones, ECoG can also map important functional areas of the brain, such as motor, language, and sensory areas {To isolate the epileptic foci because these are the areas responsible for our daily activity like moving the limbs , feeling the sense and speech } disrupting these areas could lead to permanent neurological deficits.
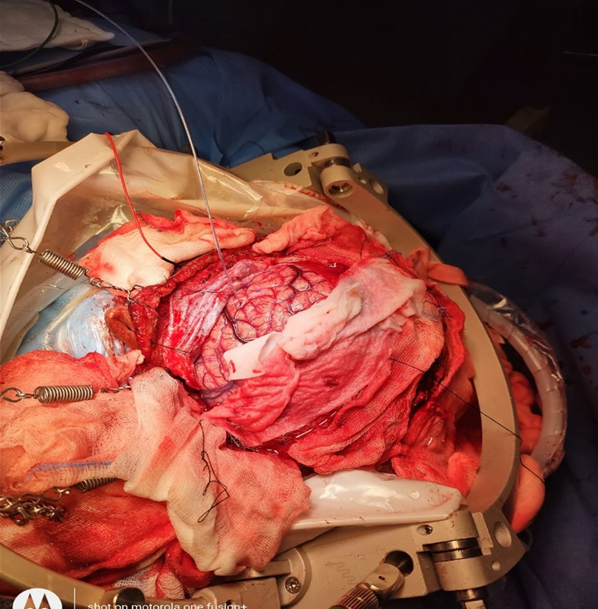
Figure.

In this image subcortical motor fiber being stimulated to see how much close to the CST fiber while disconnecting the pre-post central gyrus to isolate the epileptic form discharges .
Perioperative Decision Making.
Electrocorticogram being used intraoperatively to make real time decisions about the extent of tissue resection.
Cortical Recording.

Post resection.

Bottom 2 channel showing artifact because not touched with tissue.
Depth Recording .
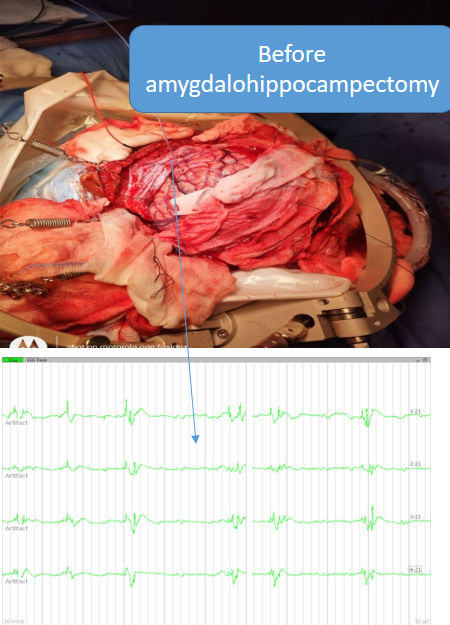
Post amygdalohippocampectomy
How to document the Grid and depth recording while procedure being performed .
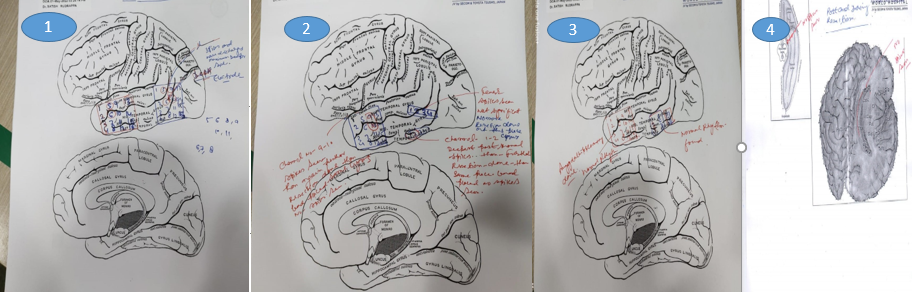
In this image showing red circle is area of epileptic discharges and blue one as a marked normal tissue of brain.
How to setup.
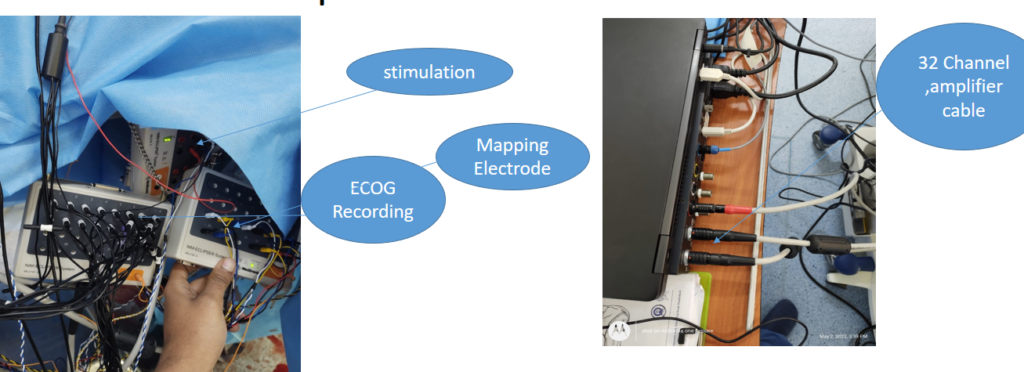
we use at least 32 channel amplifier like 16 for ECOG and another 16 for mapping .
When recording electrocorticography (ECoG) during epilepsy surgery, it's important to use
anesthesia drugs that minimize interference with brain activity while maintaining patient
safety.
What is the role of Anesthetist while epilepsy surgery being performed ?.
Propofol.
- Propofol is a commonly used intravenous anesthetic that provides rapid induction and recovery with minimal residual effects. It has a relatively short duration of action, making it suitable for short-term anesthesia during ECoG recording. Propofol is known for its ability to maintain stable hemodynamics and cerebral blood flow, making it a preferred choice for neurosurgical procedures. {Note- the dose of this drug should be as much possible minimum and constant because act on GABA Receptor and also avoid bolus during procedure.}
Remifentanil.
- Remifentanil is a short-acting opioid analgesic commonly used as an adjunct to general anesthesia. It provides potent analgesia and blunts sympathetic responses to surgical stimuli. When used in combination with other anesthesia agents such as propofol remifentanil can help maintain stable hemodynamics and anesthesia depth during Electrocorticography recording.
Dexmedetomidine.
- Dexmedetomidine is a sedative agent with analgesic properties that acts primarily through alpha-2 adrenergic receptors. It provides sedation and anxiolysis without significant respiratory depression. Dexmedetomidine is often used as an adjunct to general anesthesia or as a primary sedative agent for procedures where spontaneous ventilation is desired, such as Electrocorticography recording in epilepsy surgery.
These anesthesia drugs are chosen based on their pharmacokinetic properties, safety profile,
and minimal interference with ECoG recordings.
Electrocorticography offers higher spatial resolution because the electrodes are closer to the brain tissue.
How many minimum channels are required for recording?
What kind of metal usually preferable for ECOG electrode.
Why documentations are important.
Related this article.
https://neurointraoperative.com/wp-admin/post.php?post=1897&action=edit

Merely a smiling visitant here to share the love (:, btw great pattern.