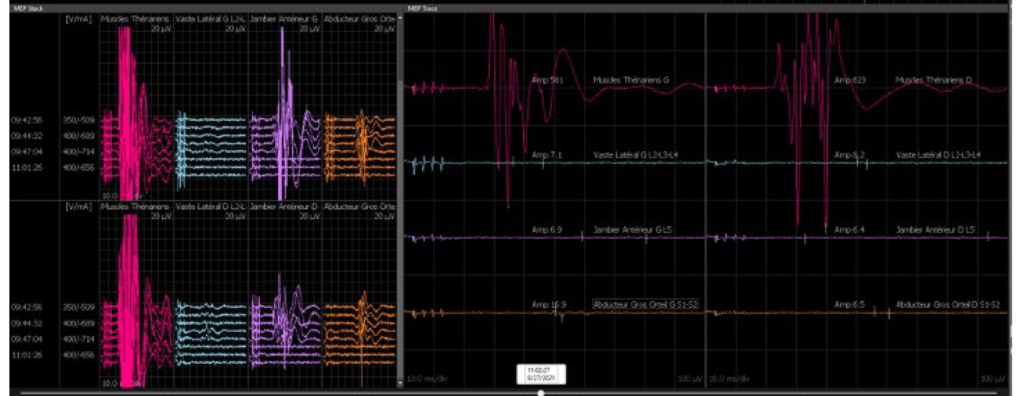
Fading of MEPs.
- While working on long spine surgeries, such as those for metastasis vertebrectomy, scoliosis or other complex tumor spine or spinal deformities, transcranial electrical motor evoked potentials [TCeMEPs] are commonly monitored to assess the functional integrity of the spinal cord and motor pathways {Descending tract}. A fading of MEPs, or a decrease in their amplitude or consistency, can be a concerning sign indicating potential injury or compromise to these pathways.

Intraoperative-Monitoring and Interpretation their signals-
- Changes of Baseline {Amplitude-phase}- Take a final baseline MEPs before starting the surgery after wear of muscle relaxant affect though TOF Monitor .Continuous monitoring should show changes in real-time. A fading of MEPs or decline in MEPs could indicate potential spinal cord compromise. { note- True fade of signals means will show drop of amplitude and reduce number of phases from the surgical side, like control should be preserve ie, while monitoring lower extremity so here upper limbs MEP should not change from the down} .
Baseline of MEPs.

Signal drop – fading of MEPs.
Pitfall- Ensure that the equipment and electrodes are functioning correctly. Sometimes, technical issues can mimic real changes in MEP signals.
Procedure related [or other] of Fading–
- Mechanical Compression- Surgical retraction or positioning might be compressing the spinal cord or nerves.
- Vascular related Issues– Reduction of blood flow or ischemia to the spinal cord due to pressure on blood vessels or changes in perfusion.
- Iatrogenic injury- Procedure related manipulation or instrumentation that impacts the direct spinal cord or nerves.
- Electrolyte Imbalance: Changes in patient physiology, such as electrolyte imbalances, can affect MEP readings so in this case possibility of {False positive -will decline of signals globally}.
What are the necessary Actions for Immediately-
- Notify the Surgeon: If MEPs are fading, it’s crucial to alert the surgical team immediately. They can assess the surgical field and adjust their approach as needed.
- Review Technique: Ensure that stimulation parameters and electrode placement are optimal. Recheck the connections and settings of the neuromonitoring equipment.
What to be done/Intervention-
- Adjust Surgical Approach: If there’s a direct impact or compression, the surgical team might need to adjust instrumentation part as well/retraction .
- Medications: Administer medications as solumedrol to reduce the cord inflammation along with improve spinal cord perfusion or address any identified issues.
Anesthesia and TCEMEPs–
Types of Anesthetic Agents –
- General Anesthetics: Agents like propofol, sevoflurane, or desflurane can affect the central nervous system and potentially reduce the amplitude or quality of MEPs. For instance, sevoflurane and desflurane are known to depress motor pathways at high concentrations.
- Propofol is preferable TIVA drug along with remifentanil.
- Neuromuscular Blockers: While not typically used during MEP monitoring, neuromuscular blockers can affect muscle responses and might be inadvertently administered.
Depth of Anesthesia–
- A Overdose of drugs- Deep anesthesia levels usually suppress MEPs by affecting the brain’s ability to generate motor responses. This suppression is generally reversible upon adjusting the anesthetic depth. {Note sodium current channel should not be completely block with very high dose of drug like in intact neurologically patient acceptable target of propofol is 120-150mcg/kg/min, if you go beyond 250mcg/kg/min than this TIVA drug also will depress the signals}.
Anesthetic Protocols–
Perioperative-Adjustments– Anesthesiologists may need to adjust the anesthetic regimen to balance the need for patient sedation through BIS monitoring , with the need for accurate neurophysiological monitoring which means signals should not get compromised.
Managing Fade MEP Due to Anesthesia–
Monitoring of Anesthesia-
- Keep Track of Anesthetic Levels: Regularly monitor and adjust the levels of anesthetic agents to avoid excessive suppression of MEPs. Ensure the anesthetic plan is optimized for maintaining MEP signal quality.
- Coordinate with Anesthesia Team–
- Communication: Maintain close communication with the anesthesia team. Alert them immediately if you notice changes in MEPs that might be related to anesthesia.
- Adjustments regular rate of infusion drug- The anesthesia team can modify the drug dosages
or switch agents if needed to improve MEP responsiveness.
Evaluate and Document–
- Document Observations: Record any changes in MEP/ fading of MEPs along with potential anesthetic adjustments made.
- Reassess Frequently: Regularly reassess the MEPs in relation to changes in anesthesia to ensure accurate interpretation of potential issues. { To avoid false positive and false negative}.

- Addressing fading of MEPs promptly is crucial to minimize the risk of postoperative neurological deficits. The key is a collaborative approach between the surgical team and the neuromonitoring specialists to ensure the best possible outcome for the patient.
- By working closely with the anesthesia team and carefully managing anesthetic agents, you can minimize the impact on MEPs and ensure effective monitoring throughout long spine surgeries.
Related to this article.
https://neurointraoperative.com/wp-admin/post.php?post=1849&action=edit

1 thought on “A fading of MEPs, or a decrease in their amplitude.”