Interventions in or around the brainstem.
- The risk of iatrogenic damage is very high in surgical intervention, However surgical techniques and intraoperative neuromonitoring (ION) have evolved sufficiently to increase the likelihood of successful functional outcomes in many patients.
Introduction.
- Surgery related to lesions in or around the brainstem represents one of the most challenging procedures in neurosurgery and requires a detailed understanding of the microsurgical and functional anatomy.
Previous .
- In the past due to the high risk of severe postoperative neurological deficits, this surgery was restricted to biopsy procedures only.
Now the differences with IONM.
- The development of intraoperative neurophysiology over the last two decades, together with the emergence of more refined imaging techniques, better surgical instruments, and more effective Neuro-Anesthesia and postoperative intensive care, have increased the feasibility and safety of brainstem surgery.
Let's start with Cranial Nerves Monitoring.
What are the challenges to the Neuro-Surgeon.
Compression related displacement of classical anatomical landmarks such as the facial colliculus or the striae medullaris is a common difficulty for neurosurgeons, Even when the anatomy is not significantly distorted, the identification of areas overlapping the lower cranial nerve motor nuclei (CMN) can represent a major challenge.
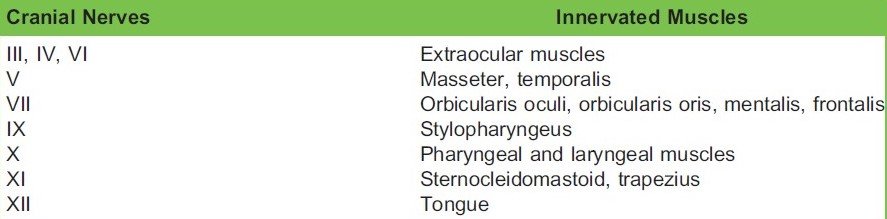
Intraoperative neurophysiological mapping technique can be used to identified the functional structures such as the CMN of cranial nerves III, IV, V,VI, VII, IX, X, XI and XII .
Direct electrical stimulation of the brainstem may be invaluable for choosing the safest approach for intrinsic brainstem tumors.
Mapping techniques should never replace monitoring techniques, we consider three main groups of neurophysiologic techniques that may help monitoring the brainstem functional integrity. Mapping, which provides rapid anatomical identification of neural structures by electrical stimulation with a hand-held probe, but monitoring which provides real-time information about the functional integrity of the nervous tissue along with anatomical preservation and intraoperative testing of the brainstem reflexes.
What we found here .
Mapping and monitoring techniques complement to each other and should be used together during challenging surgical procedures such as tumor resection in or around the brainstem.
So here multi modalities can be used to assess the function and anatomical preservation .
- Triggered Electromyography {TEMG} the only modality to asses the function of oculomotor nerve cranial nerves {III,IV,VI}
- Corticobulbar Transcranial Electrical Motor Evoked Potentials {CTEMEP}, and Triggered Electromyography {TEMG} can be used together to assess the function and long term anatomical preservation of CMN of cranial nerves V, VII, IX, X, XI and XII.

Cranial nerve monitoring will depend on lesion like if its medullaris level than Lower cranial nerves {LCNs} and if its on mid brain than upper cranial nerves like II ,III, etc , For monitoring cranial nerves II which is your optic tract so here Visual Evoked potential {VEP} will be useful , and if its on pons and upper medulla than Blink reflex VII ,VIII can be monitored .
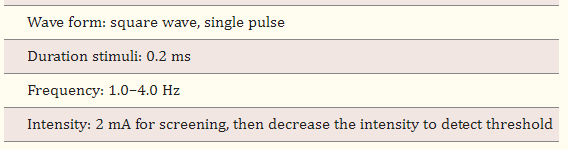
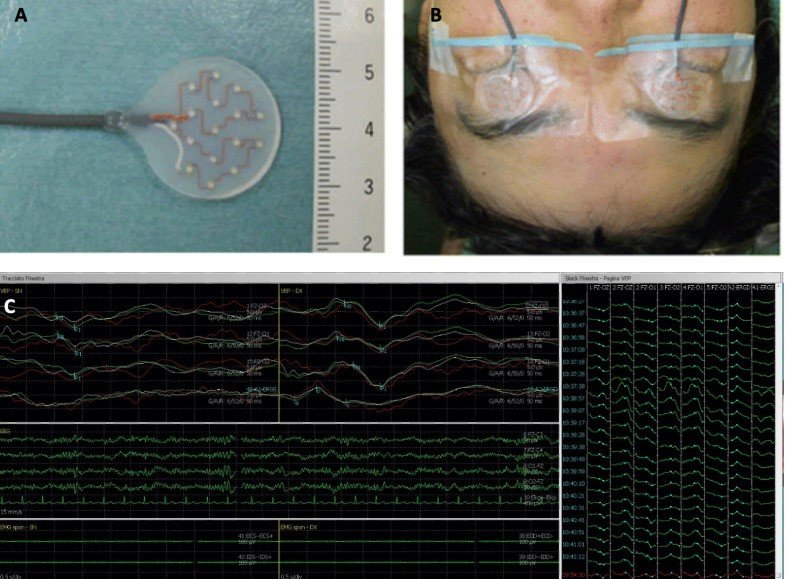
Stimulation parameters .
Concentric probe will be very much useful to stimulate the exactly targeted tissue and this probe does not spread much current because distance between two pole cathode and anode is 2-3 millimeter only.
Other suction monopolar probe can be used incase of functional neural structures not very much visible due to tumor overlap and anatomical distorted. {only drawback if this probe its spreads current , possibility will be there volume conduction but this problems can be resolves, so here keep low intensity of current like 0.3-0.5 milliampere to identify the functional tissue than concentric can be preferred to identify exact location}.
The blink reflex
- Is a neurophysiological response involving the involuntary contraction of the muscles that control eyelid movement in response to a sensory stimulus. It is a protective mechanism designed to shield the eyes from potential harm, such as foreign objects or sudden bright lights.
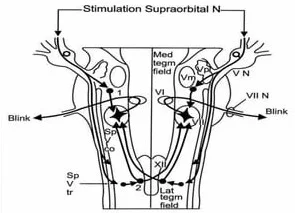
The blink reflex pathway involves several neural components.
Sensory Input.
- The trigeminal nerve (cranial nerve V) carries sensory information from the face, including the area around the eyes, to the brainstem. Specifically, the ophthalmic branch of the trigeminal nerve (V1) innervates the cornea and conjunctiva, providing sensory input for the blink reflex.
Brainstem Processing.
- The sensory information is relayed to the brainstem, particularly the trigeminal sensory nucleus, which is located in the pons. Here, the incoming signals are processed and integrated.
Motor Output.
- From the brainstem, motor signals are sent out via the facial nerve (cranial nerve VII) to the orbicularis oculi muscles, which are responsible for closing the eyelids. The facial nerve nucleus, specifically the facial motor nucleus in the pons, is involved in coordinating this motor response.
Stimulation:
- The sensory component of the blink reflex is typically elicited by applying a mild electrical stimulus to the supraorbital the area around the eye. This can be done using a twisted needle electrode at 45 degree.
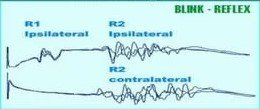
Recording.
- Twisted needle electromyography (EMG) electrodes are placed on the skin overlying the orbicularis oculi muscles, which are responsible for closing the eyelids. These electrodes detect the electrical activity generated by the muscle contractions.

Analysis.
- The EMG activity can be recorded from the orbicularis oculi muscles is analyzed to assess the latency (time delay) and amplitude of the blink reflex response. Latency refers to the time interval between the stimulus application and the onset of the muscle response, while amplitude reflects the strength of the muscle contraction.
Comparison.
- The latency and amplitude of the blink reflex response are compared to established norms or to the contralateral side (if applicable) to identify any abnormalities. Changes in latency or amplitude may indicate surgery related dysfunction along with trigeminal to facial nerve pathways.
{Important Note Blink Reflex modality only will assess the function of Pons , If lesion like Cavernoma ,Hemangioblastomas or other type of abnormality in brain-stem or around the brain-stem this single modality will not be very much helpful because blink reflex pathway does not cover from the mid brain to medulla, only covers pons}
Visual Evoked Potential {VEP}
VEP measures the functional integrity of the optic pathways from the retina to the brain’s visual cortex in response to light stimulus. Visual stimulus is converted into nerve signals in the retina. These signals are transmitted via the optic pathway to the brain, from the retina to the optic nerve, optic chiasma, optic tract, lateral geniculate body, optic radiation, and visual cortex occipital lobe.
Interpreting intraoperative VEP involves analyzing the characteristics of the evoked potentials recorded during the procedure. Here are some key aspects of interpretation
Amplitude.
- The amplitude of the VEP waveform reflects the strength of the neural response generated in the visual cortex in response to the visual stimulus. A decrease in VEP amplitude compared to baseline recordings may indicate impairment or disruption of the visual pathway.
Latency.
- The latency of the VEP waveform refers to the time interval between the presentation of the visual stimulus and the peak of the evoked potential. Prolongation of VEP latency may suggest delayed conduction along the visual pathway, which could be indicative of early nerve damage or dysfunction.
Comparison.
- Intraoperative VEP recordings are often compared to baseline or preoperative VEP measurements obtained from the patient to assess any changes or abnormalities during the surgery. Additionally comparisons may be made between different stages of the procedure to evaluate the impact of surgical manipulation on visual pathway function.
Brief about of anesthesia drugs .
Visual pathway contains multiple synapses , time delayed between two synapse is 500 micro-second that is the why avoid GABAergic drugs and its affects impairs neurotransmission and inhibiting synaptic transmission.
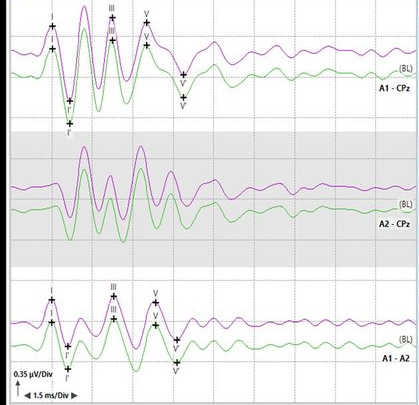
For VIIIth this nerve emerging from the lower pons and upper medulla to assess the function of this nerve Brainstem Auditory Evoked Potential {BAEP} modality can be used .
BAEP monitors the function of the auditory nerve and auditory pathways in the brainstem. The auditory signal travels from the cochlear hair cell to the primary auditory cortex via the vestibulocochlear nerve, superior olivary complex, lateral lemniscus, inferior colliculus, and medial geniculate.
interpretation.
usually we follow as per universal methods , inter-pick Latency delayed 10% and amplitude drop 50%.

Corticospinal tract and cerebral peduncle.
Injury to the corticospinal tract (CST) is a major concern when performing surgery close to the cerebral peduncle or the ventral part of the medulla. Brainstem surgery has benefited significantly from the introduction of techniques for the intraoperative recording of Motor Evoked Potentials {MEPs}. MEPs can be used to monitor the integrity of the motor pathways in the brainstem. Stimulating the motor cortex and peripheral nerves and recording muscle responses allow the surgical team to assess the functional status of the motor pathways during surgery.
Signal fade.
- Changes in MEP can indicate potential damage to the motor pathways in the brainstem, such as compression or injury.
- Prompt detection of such changes can alert the surgical team to take immediate corrective actions to prevent permanent neurological deficits.
- MEP monitoring allows to identifying the optimal surgical approach and monitoring the manipulation of critical structures around and in the brainstem to minimize the risk of motor deficits.
Role of SSEPs in Brainstem Surgery.
- If approaching from the posterior side or, like far lateral craniotomy {Park-Bench} somatosensory evoked potentials {SSEPs} are useful to monitor the integrity of the sensory pathways in the brainstem and other regions of the nervous system.
- By stimulating peripheral nerves and recording the sensory responses along the neural pathways, SSEPs provide valuable information on the functional status of sensory pathways during surgery because its a continuous monitoring and does not disturb surgical field.
Conclusion.
As we know previous era there was limitation of monitoring and mapping technique .
Now current era well developed all modalities and intraoperatively identifying all major and minor functional neural structures, while manipulating structures with any angle.
Neurophysiological monitoring subject provides real-time feedback to surgeons, allowing them to adjust their approach to minimize the risk of neurological deficits during brainstem cavernoma along with other type of tumor surgery.
Multimodality technique helps in identifying potential complications early and improving patient outcomes.
Here sharing my Experiences in this type of complicated procedure.
Case Report.
Cervico-Medullary hemangioblastoma.
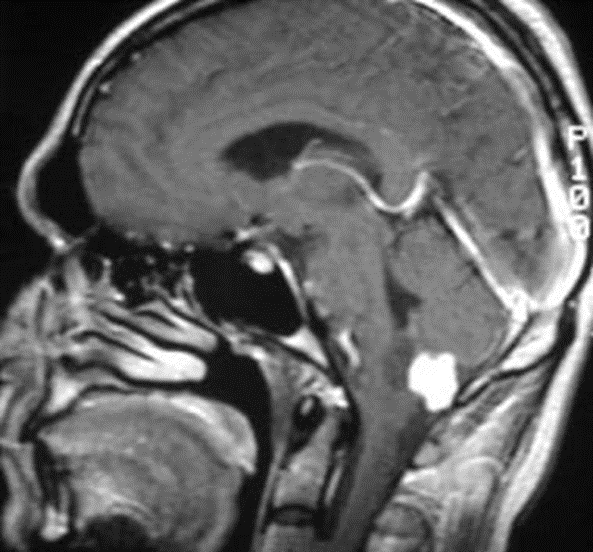
History
22 year old Female.
Gradually increasing weakness of RT side of the body it was followed by difficulty in deglutition .
No H/O Seizure /vomiting/fever.
Examination.
- Conscious, Following commands
- Vitals Stable
- .Chest, P/A – NAD
- .Higher mental functions – Normal
- .GCS – E4V5M6
- .Pupil- B/L RTL 2+
- .Cranial Nerves – Normal –Except IX-X .
- .Voice Husky ,Gag Reflex-↓
- .Power RT-U/L,L/L 3/5
- LT-U/L,L/L 4/5.
- Planter B/L Flexor Response.
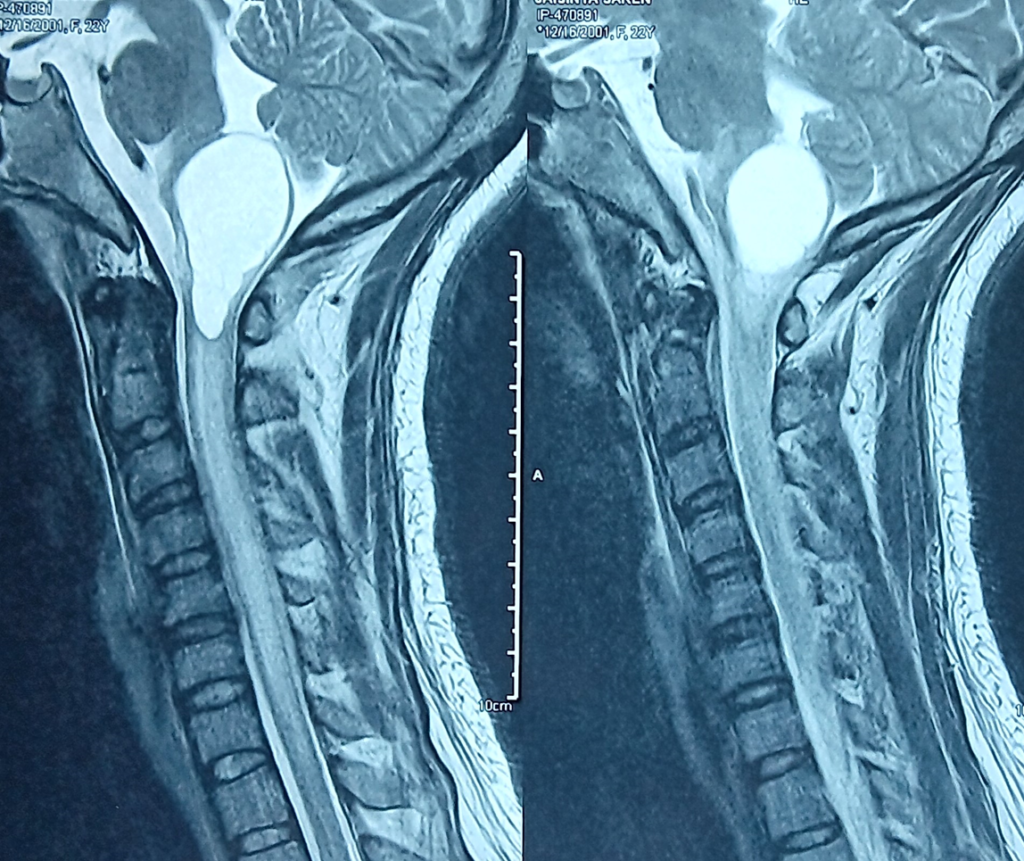
Scan.
Cystic lesion with a mural nodule at the cervico-medullary junction, with significant mass effect on the medulla.

Axial Section.
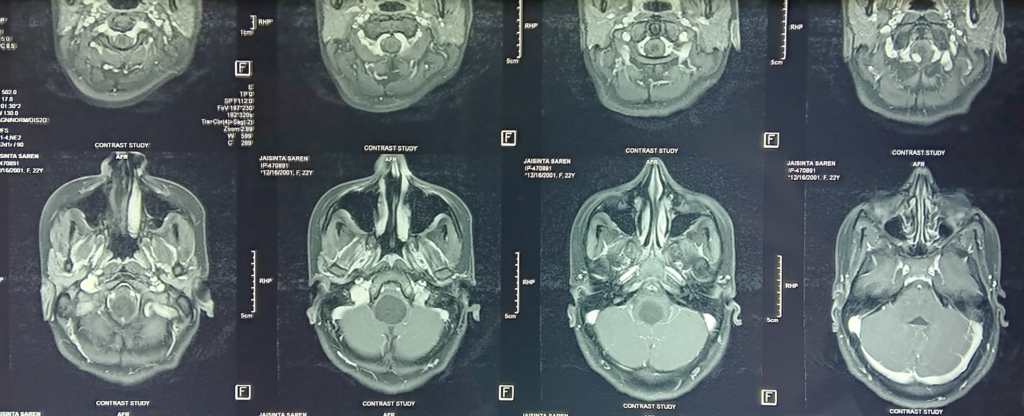
MRI of c- spine: significant edema in the cervical cord, mural nodule at cervico-medullary junction
Plan.
Rt. Far lateral craniotomy and excision of lesion under intraoperative neurophysiological monitoring GA.

Baseline MEPs.
Due to weakness baseline signal was weak on the Right side.
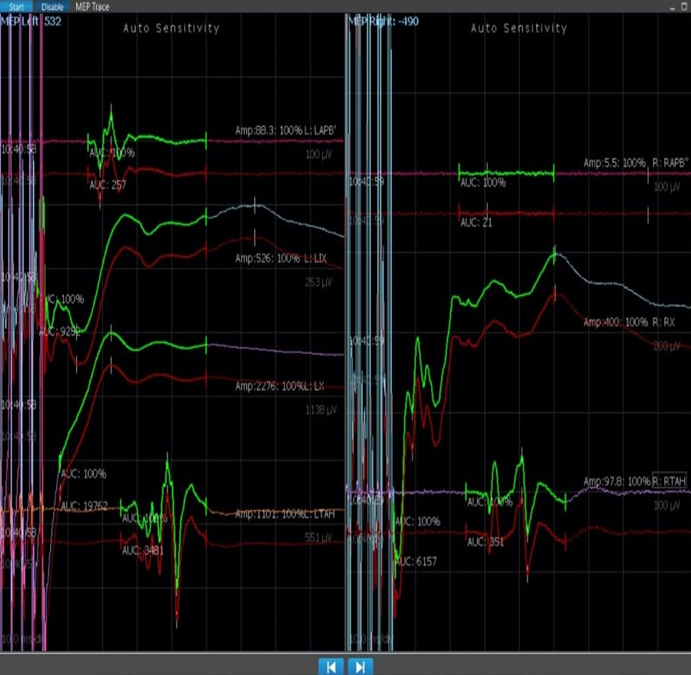
Continuous Monitoring throughout the procedure.
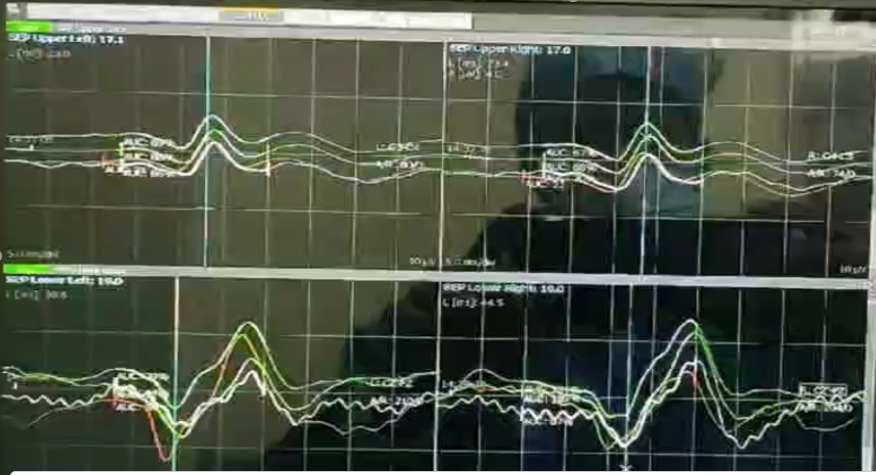
When tumorectomy about to complete .
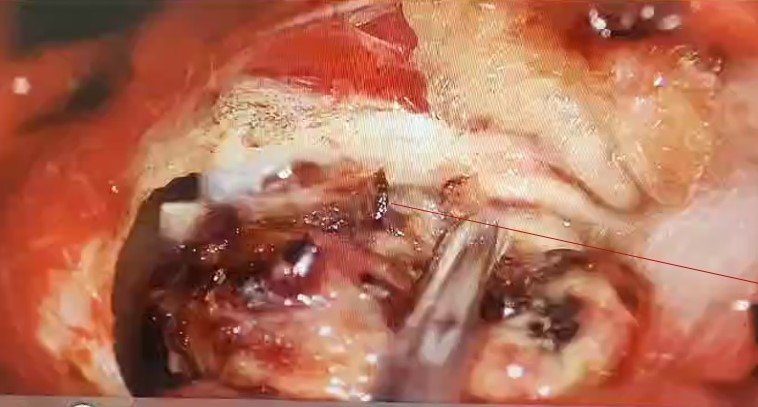
Signal got improved .
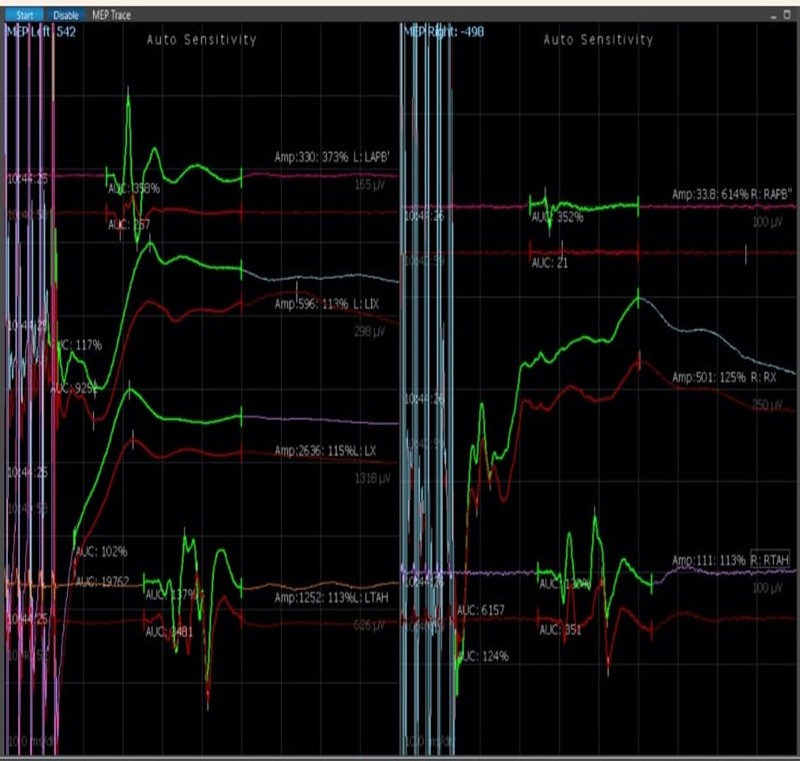
As per signal improvement patient clinically also improved like muscle power ,Gag reflex and also improved her husky voice.
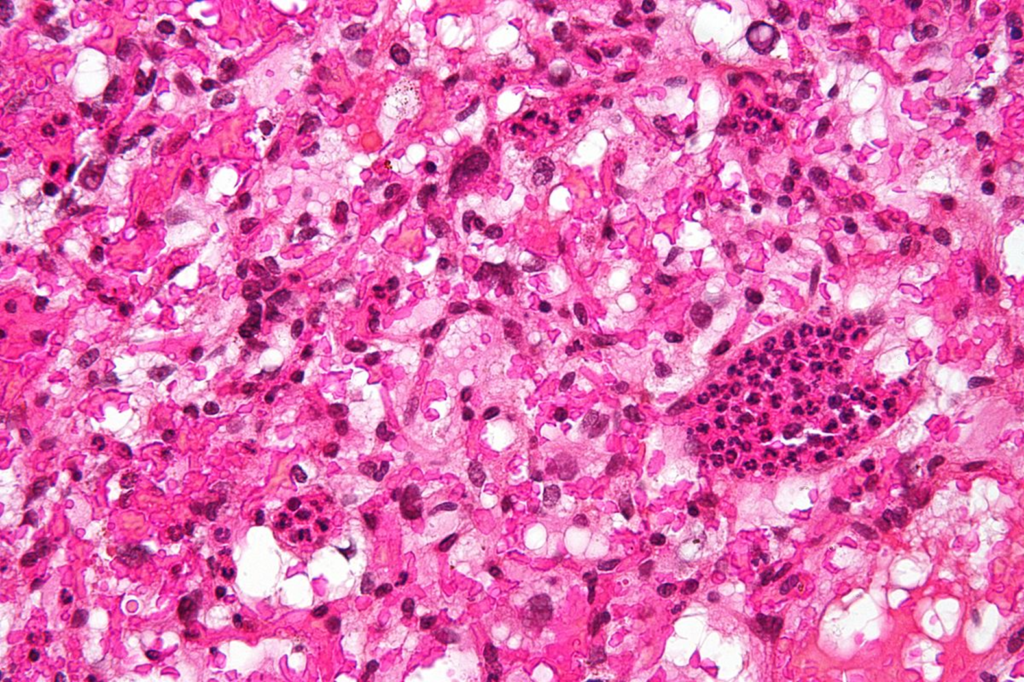
Her Histopathology report showed Hemangioblastoma, CNS WHO grade 1.

This case operated by senior consultant .
Dr. Debarshi Chatterjee is a Neurosurgeon at The Institute of Neurosciences, Kolkata
- Specialty: Neurosurgery
- Qualification: MBBS, MS, MCh Consultant Neurosurgeon
- I hope this article will help you more to understand the concept is really brainstem surgery are safe under this subject , IONM not only prevent neurological deficits it gives confident to the surgical team and also controls surgeon’s Heart palpitations .
Related to this article.
https://neurointraoperative.com/wp-admin/post.php?post=1553&action=edit
https://www.sciencedirect.com/science/article/abs/pii/B9780128198261000211
Question.
- What is the role of Intraoperative Neurophysiological Monitoring IONM in high cervico-medullary junction tumors/Brain-stem?
- Can we use all type of modality what i had written in this Article or according lesion/pathology/tumors?
- As we are surgical Neurophysiologist should we understand the MRI/CT scan before surgery?
- How much risk while intervention around the brain-stem?
- What kind of tumor is hemangioblastoma?.

2 thoughts on “Mapping and Monitoring Functional Integrity of the Brainstem.”