Introduction about Selective Dorsal Rhizotomy SDR for spastic cerebral palsy.
Cerebral palsy is a major neurological problem in children It occurs in 1 of 500 live births and inflicts lifelong disabilities on those with the disorder. Several factors contributing to the disabilities of patients with CP is spasticity.
This condition affects nearly 80% of patients with CP, and once fully developed and it never resolves spontaneously.
It hinders motor tasks in activities of daily living and also causes muscle contractures and orthopedic deformities in growing children.
How surgical procedure and Intraoperative neurophysiological monitoring (IONM) helps to make quality of life .
Selective Dorsal Rhizotomy is a well-established surgical procedure for improving lower extremity spasticity in children with cerebral palsy.
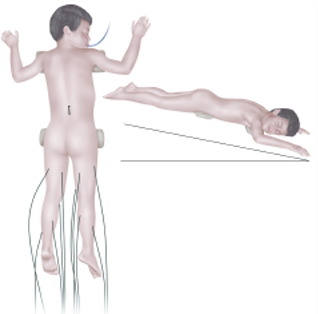
The standard technique requires an L1–S1 or L2-S1 laminectomy or laminoplasty for visualization of all dorsal nerve roots exiting at their respective foramina. During the SDR procedure, the neurosurgeon selectively cuts specific sensory nerve roots in the spinal cord to reduce the abnormal sensory input that leads to spasticity.
Neurophysiological Monitoring involves the continuous monitoring of the peripheral nervous system’s functional integrity during surgery. It helps the surgical team assess the status of neural structures in real-time, identify any potential damage, and make adjustments to minimize adverse outcomes.
In the term of Selective Dorsal Rhizotomy for Cerebral Palsy , Neuromonitoring several important facts.
Identification of Sensory Nerve Roots.
Neuromonitoring helps the surgeon accurately identify the sensory nerve roots responsible for transmitting abnormal signals contributing to spasticity.
By accurately localizing these nerve roots, the surgeon can selectively target them for rhizotomy while preserving other critical neural elements,{Motor}.

Choice of muscles to place to recording electrodes. {Rhizotomy}
Iliopsoas.
Rectus femoris
Hamstring {Biceps femoris}
Tibialis Anterior
Gastrocnemius.
Abductor hallucis brevis.
Extensor hallucis longus
Extensor digitorum brevis.
Choice of modalities .{Rhizotomy}
In this type of procedure, The primary role of Trigger Electromyography to assess the function of peripheral nerve ,while separating dorsal and ventral nerve roots .
Stimulation parameters.{Rhizotomy}
The frequency can vary depending on the specific nerves being targeted and the response being evaluated. Most important modalities are the Electromyography triggered (TEMG) with standard single pulse method and with 50-Hz train method, secondary transcranial motor evoked potentials (TcMEPs), and somatosensory evoked potentials (SSEPs)
TEMG contains two components (described below): (A) Identification of the threshold of each sensory root (single pulse technique). (B) 50-Hz train stimulation to the rootlets. Grading is performed thoroughly for sectioning only after completing both components of TEMGs.
The threshold of the current, usually measured in milli-amperes, for each dorsal sensory root is identified by placing the root over two hooks of rhizotomy
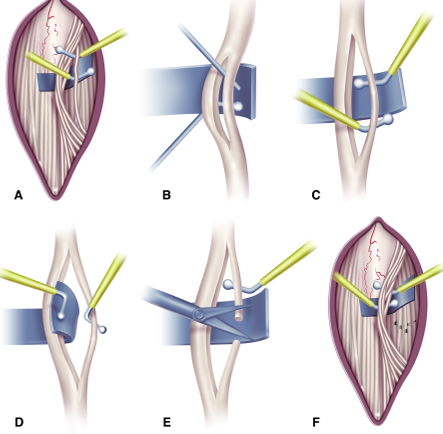
In this figure Illustrations depicting the procedure.
A: The L-2 dorsal root is easily identified. In an attempt to identify theseroots for L3–S2, all the dorsal roots are spread over the Silastic sheet and grouped into presumed individual roots. Then
the innervation pattern of each dorsal root is examined by assessing EMG responses to electrical stimulation with a threshold voltage.
B: With a Scheer needle, each dorsal root is subdivided into three to five rootlet fascicles, which are
subjected to EMG testing.
C: Stimulation of an L-2 rootlet fascicle elicits an unsustained discharge to a train of tetanic stimuli.
D: The rootlet is therefore spared from sectioning and placed behind the Silastic sheet.
E: Stimulation of a rootlet fascicle elicits sustained discharges from multiple muscles, and the rootlet is therefore sectioned.
F: The rootlets spared from sectioning are under the Silastic sheet, and the roots to be tested are on top of the sheet.
Note that EMG testing and sectioning of the dorsal roots are completed caudal to the conus medullaris
standard Park and Phillips grading criteria.

Putting the patient’s clinical presentation into consideration, the rootlets generating a response activity of 0, 1+, or 2+ are left intact, while rootlets generating a response activity of 3+ or 4+ are sectioned.
The desirable sectioning percentage at each segment level is 40–60% with the exception of L4 level, where only up to 50% rootlet sectioning can be performed or 60% but this percentage also depend on surgeon , in order to avoid 80%-90% causing permanent sensory loss postoperatively and also to minimize complications of muscle function.
Value of Free run Electromyography.{Rhizotomy}
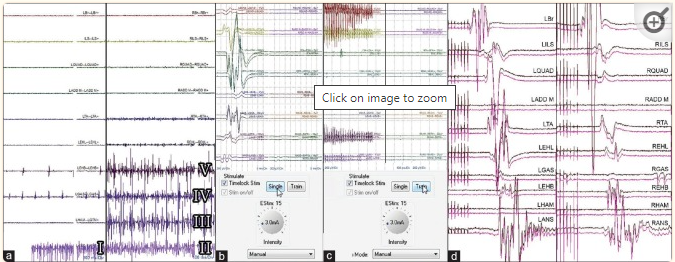
Free running electromyographies showing root irritation at various cauda equina levels while the surgeon is working on the lower lumbar and sacral roots: anal sphincter irritation (I and II), right hamstring muscles irritation (III), right gastrocnemius muscle irritation (IV), and right extensor hallucis brevis irritation (V), the remaining muscles show no root irritation (a). Identifying root threshold with single pulse technique showing triggered electromyogram responses at 3 mA on the left side (b). Identifying and grading the rootlet with 50-Hz train technique showing sustained discharges on the left side at 3 mA (c). Transcranial motor evoked potentials showing the presence of compound muscle action potentials confirming the integrity of specific motor roots (d)
MEP Monitoring Corticospinal Tracts Is really useful?.{Rhizotomy}
For gross conduction corticospinal tracts are vital neural pathways responsible for motor control. IONM allows the surgical team to monitor the integrity of these tracts during the procedure. Preservation of the motor nerve roots along with corticospinal tracts is essential for maintaining motor function and preventing complications such as weakness or paralysis.
Aim to Neurological Changes:{Rhizotomy}
Monitoring provides real-time feedback on neurological function, Monitoring of electromyography {EMG}, sensory and motor evoked potentials, responses, gives significant alterations in these parameters may indicate potential nerve injury or compromise, prompting the surgeon to adjust the procedure accordingly.
Surgical Outcomes.{Rhizotomy}
By guiding surgical decision-making and minimizing the risk of neurological injury, IONM helps optimize the overall outcomes of SDR for CP. It allows for a more precise and tailored approach, increasing the likelihood of achieving the desired reduction in spasticity while preserving motor function and minimizing complications.
Conclusion .
The integration of Neurophysiological Monitoring into SDR procedures for spastic cerebral palsy enhances the safety and efficacy of the surgery, ultimately improving outcomes for patients with CP. It allows neurosurgeons to perform targeted interventions while minimizing the risk of adverse neurological effects, leading to improved functional outcomes and quality of life for individuals undergoing this treatment.
Related to this article.
https://neurointraoperative.com/wp-admin/post.php?post=1468&action=edit
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5532931
Question.
- When can be done Selective Dorsal Rhizotomy in CP child?.
- Which modality is useful for this type of surgery Intraoperative neurophysiological monitoring IONM?.
- Motor Evoked Potentials are useful?
- What is the Grading system?
- This procedure can be done in supine position?.

Very good illustration, thanks sir
Iam also very happy you guys are liking my article.