Introduction of TCEMEP.
- Iatrogenic injuries are an undesired consequence of surgery, yet iatrogenic injuries to the motor system are much more devastating to a patient’s quality of life than most injuries to the sensory system.
- Generally an injury to the spinal cord will be most likely be picked up by somatosensory evoked potentials (SSEPs), yet a focal injury to the anterior spinal artery (ASA) may be missed There is a lot of evidence in the literature describing selective injury to the anterolateral columns sparing dorsal columns with preserved SSEPs .
- The inclusions of transcranial electrical motor evoked potentials (TCEMEPs) to the intraoperative monitoring toolbox can help to confirm/prevent selective lesions to the anterolateral columns of the spinal cord. Yet TCEMEPs are not without their limitations. Even with these limitations, proper application and interpretation of TCEMEP data can be a significant adjunct in reducing iatrogenic injury during surgery.
Anatomy and Physiology of the Motor System Regarding TCEMEP.
Before doing and interpreting the waveform signals of TCEMEP.
- The motor system is a complex combination of neural sub systems existing in both the central and peripheral parts of the nervous system. It is important to realize that artificial stimulation most likely activates many different cortical fibers, while TCEMEP monitoring techniques only record responses from a small portion of them figure 1.
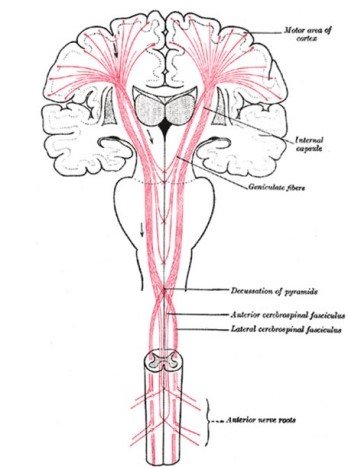
Figure 1– Multiple areas of the cortex are involved in motor movements. In addition to the cortex, there also exist multiple subcortical areas. During artificial simulation under anesthetics, the corticospinal fibers are the main carriers of that stimulation information to the alpha motor neurons in the spine. Even though the stimulation will activate fibers from other areas, this information is usually not passed due to the synaptic junctions between the other areas and the corticospinal tract which under anesthesia are shut down for the most part.
- The primary anatomic structure of the MEPs is the Betz cell in layer five of the motor cortex and its axons in the Corticospinal Tract {CST} and corticobulbar tract (CBT) (upper motor neuron), the spinal or α-motor neuron (αMN) and its axon (lower motor neuron), and the end organ (muscle).
- There also exist indirect corticofugal motor pathways not projecting directly to the spinal cord, but indirectly having interruption on their descending route to the αMN.
- The primary motor cortex, where the CST fibers originate, is located in the precentral gyrus and is primarily responsible for fine voluntary movement. This area of the cortex receives information from multiple cortical areas which include the extrapyramidal system (areas such as the basal ganglia and cerebellum) and sensory areas including somatosensory, visual, auditory, both parietal, and frontal cortices.
- The primary motor cortex has a map of the body or homunculus, with the head located laterally on the cortex and the leg located within the interhemispheric fissure.
- The primary pathways that we are concerned with when monitoring TCEMEP during surgery are depicted in Figure 2 .
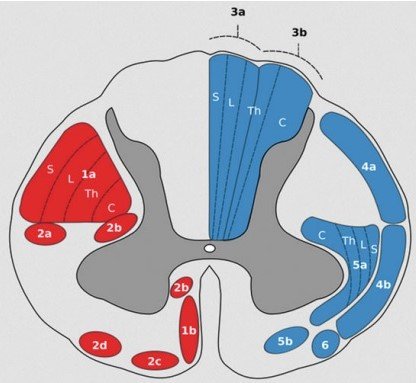
Figure 2 The corticospinal and corticobulbar pathways. The pyramidal fibers originate in the motor cortex and traverse through the internal capsule. At this point the corticobulbar fibers are medial and synapse on the secondary axons in the brainstem. Most corticospinal fibers decussate in the medulla and travel in the lateral corticospinal columns to synapse at the alpha motor neurons located in the anterior horn of the spinal gray matter. The lateral corticospinal tract (1a in the figure) shows a lateral to medial homunculus with the sacral region being most lateral and the cervical region being most medial. Region 1b is the anterior corticospinal tract in the spinal cord. T
- At the surface of the cortex are six layers of gray matter. Each functional area of the brain has different proportions of each of these six layers, yet the basic six layer structure is the same throughout the cortex. Each area of the cortex is defined based on its specific cytoarchitecture and neural organization.
- The nomenclature used for this differentiation is known as a Brodmann area Interestingly each Brodmann area generally corresponds to a specific functional area, even though the original differentiation was purely based on its cytoarchitecture
- Generally layer 5 is the output while layer 4 is the input layer. The primary motor area (PMA), or Brodmann area 4, is located in the posterior portion of the frontal lobe just anterior to the central-sulcus (Fig. 3 ).
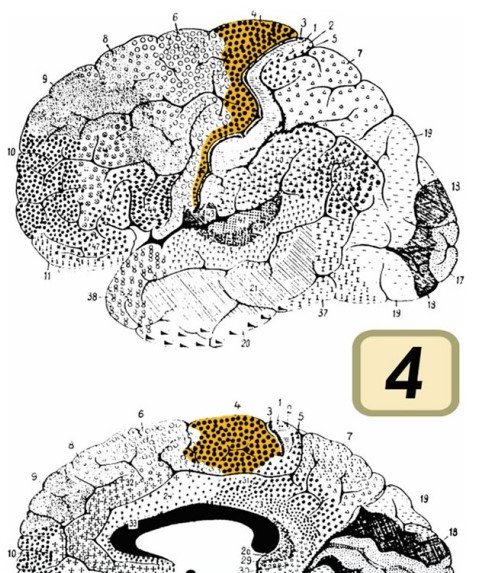
Fig. 3- Map of the cortex with all of Brodmann areas depicted. Area 4, the primary motor cortex, is highlighted . Area 4 is just anterior to the central sulcus .
- Layer 5 of the primary motor cortex contains large pyramidal cells known as Betz cells that send long axons directly to motor neurons located in the spinal cord or brainstem via the CST or Corticobulbar Tract (the combination of these two tracts is known as the pyramidal tract).
- About 60 % of the human CST fibers arises from the primary motor cortex and area 6 (premotor area and supplementary motor area) the other 40 % arises from the somatosensory cortex (areas 1, 2, and 3) and cingulate cortex (areas 23 and 24) .
- Even though all areas of the body are represented within the primary motor cortex, it appears that more proximal and axial muscle fibers in the CST have their origins in the premotor area (area 6),while the distal musculature tends to have its origin in the Primary Motor Area (area 4) .
- Since both sets of fibers are contained in the CST, stimulation used during TCEMEP-IONM will activate both of them. From the cortex the CST funnels into the anterior half of the posterior limb of the internal capsule and then travels between the thalamus and parts of the basal ganglia (striatum and globus pallidus) to the ventral portion of the cerebral peduncles (in the middle two fifths of the cerebral crus anterior portion of the cerebral peduncles).
- At this level the fibers that will eventually synapse on αMNs in the spinal cord gray matter innervate leg muscles and are lateral to fibers eventually innervating hand muscles. TCEMEP activates and record them.
- From the midbrain the CST fibers enter the pons and pass through the pontine nuclei where fibers going to the leg muscles are now located ventrolateral relative to the fibers going to the hand muscles. The CST enters the ventral part of the medulla forming part of the medullary pyramids where fibers innervating the lower limbs are located ventrolateral compared to the fibers innervating the upper limbs. TCEMEP checks conduction of these fibers.
- At the lower level of the medulla, 80–90 % of the CST decussates with most fibers entering lateral CST of the spinal cord.
- Fibers going to the lower limb muscles tend to cross more rostrally than for the upper limbs. The 10–20 % of uncrossed fibers in the anterior CST innervate αMN ending on more proximal and trunk musculature .There are about one million fibers in each CST with around 2 % of these fibers being large 11–20 μm which are known as fast conducting corticospinal fibers (conduction around 50 m/s).CST fibers for the upper limb are more medial than lower limb fibers. TCEMEP.
- The rest of the CST fibers synapse on other interneurons within the gray matter of the spinal cord. The large CST fibers are essential for eliciting MEPs. About 55 % of all CST fibers end in the cervical region with 25 % innervating the lower limbs and the rest innervates the thoracic region. It is interesting to note that the CST is not symmetric, and it appears that CST fibers that cross more anterior tend to form the larger CST in the cord whether it is the right or the left. A single αMN has over 1,000 synapses yet only around 22 dendrites thus in the awake animal generation of an action potential in the αMN is a complex process of competing systems. TCEMEP.
- In the anesthetized animal this complex system is shut down due to anesthetics. In addition to αMN CST inputs, there are inputs from interneurons driven by other CST fibers, inhibitory interneurons, Renshaw cells (which are inhibitory), sensory Ia and Ib fibers, and other descending tracts including the rubrospinal tract, vestibulospinal tract, reticulospinal tract, and tectospinal tract. Many of these presynaptic fibers synapse at many places on the αMN, instead of one point. Due to the large number of synapses, it appears that the control of the αMN is multifactorial. In the non-neurologically compromised awake human, all the synaptic inputs to a specific αMN modulate the membrane potential, thus appropriate supra-tentorial modulation appropriately depolarizes the cell.
- The CST enters the gray matter of the spinal cord in the ventral horn and fans out terminating in laminae IV through IX. Yet the largest CST fibers appear to make monosynaptic connections to the αMN in laminae IX . Most of the CST tends to synapse on interneurons, some of which being part of circuits that modulate the αMN, while others influence motor circuits such the γ-motor system. TCEMEP
- Axons from the αMN innervate muscle fibers of a single muscle. The αMN and its axon are known as the lower motor neurons. The combination of the αMN, the terminal branches of the αMN, and the muscle fibers they innervate is known as the motor unit. Each motor unit is innervated by one axon and thus only one αMN.
- Damage to either the upper motor neurons or the lower motor neurons will cause paralysis. Damage to the lower motor neuron will result in what is known as a flaccid paralysis no muscle tone and no movement.
- Damage to the upper motor neuron shows in a much more complex set of symptoms but generally includes no voluntary movement and a range of muscle tone from minimal tone to severe spasticity. TCEMEP.
Indirect damage to the motor system can arise from reducing the blood supply to the critical
structures. TCEMEP Signal changes .
- The cortex is supplied primarily by four main vessels, the two carotids and the two vertebral arteries. These four vessels supply the circle of Willis (COW) presenting connection between the carotid and vertebral arteries. The COW, with basilar artery complex, converts the flow from these four vessels into a network supply for the brain and brainstem. The middle cerebral artery (MCA) coming from the carotid artery supplies the lateral motor cortex and its descending axons.
- The anterior cerebral artery (ACA) supplies the medial parasagittal motor cortex and its descending axons originating from the motor cortex. Axons at the CST within the internal capsule are supplied by lenticulostriate branches originating from the MCA and the anterior choroidal arteries. At the level of the brainstem, the CST is supplied by branches of the vertebral and basilar arteries.
- The spinal cord is supplied by one Anterior Spinal Artery, two posterior spinal arteries (PSA),and a varying number of radicular arteries. The ASA supplies the anterior 2/3 of the spinal cord including the lateral and anterior CSTs and the ventral horn. In the adults the ASA is formed via fusion of the anterior spinal branches of the vertebral arteries, while the PSA originates from the posterior inferior cerebellar arteries .
- In the thoracic spinal cord, there is usually one large supply vessel coming from the aorta known as the artery of Adamkiewicz and two or three smaller vessels. Interestingly, in about 10% of patients this vessel enters the spine at the L1–L2level .
- This variability in supply demonstrates one of the critical needs for neuromonitoring. Normally watershed zones are most commonly at levels T1, T5, and T8–T9 where reductions of blood flow in any of the feeder vessels can cause significant ischemia at these regions ..{ Note-if injury happens this artery only – Motor Evoked potential TCEMEP will show reduction of amplitude and phase but Somatosensory Evoked Potential will remain intact because supply only motor.}
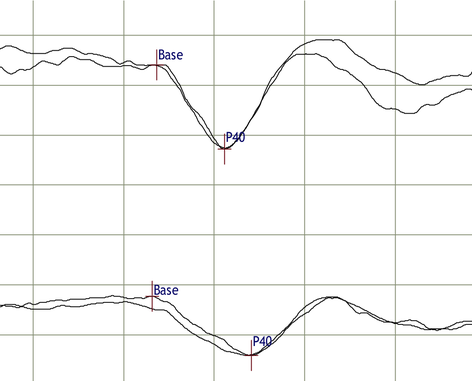
Signal changes in TCEMEP.
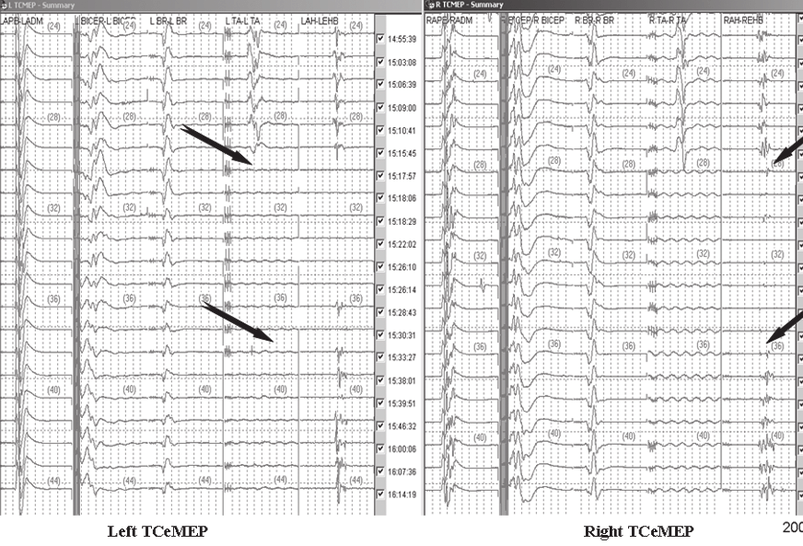
Intact SSEP.
{ I hope this article will be helpful for you to understand the physiology and anatomy of motor system while recording TCEMEP}
Related article.
https://neurointraoperative.com/wp-admin/post.php?post=1970&action=edit
https://thejns.org/downloadpdf/view/journals/neurosurg-focus/43/4/article-pE8.pdf
Question.
- How much motor fibers get decussate other side?.
- How much motor fibers remains same side?.
- which tract we monitor in MEP, Pyramidal or extrapyramidal?
- Why we should know, the theory of MEP?
- How much signal loss of MEP indicates alert?

Thank you to read the article
You have mentioned very interesting points! ps nice web site.
F*ckin’ tremendous things here. I am very glad to see your post. Thanks a lot and i am looking forward to contact you. Will you please drop me a mail?
Please maintain some decency because its a academic platform.