Neurophysiological monitoring of cervical cord function is crucial during surgeries for cervical myelopathy.
Introduction.
- Cervical spinal cord compressive myelopathy is one of the most commonly acquired cause of spinal cord dysfunction and surgery is usually the treatment of choice for those patients.
- It is important to assess cervical cord function in patients with compressive myelopathy during surgical treatment, the majority of studies are concerning the application of intraoperative transcranial electrical motor evoked potential [TCeMEP] to detect impending spinal cord damage its early warning the operating team to take action to avoid injury in cervical spine surgery.
Types of MEP baseline according to grade of myelopathy.
- The different type of perioperative MEP baselines before cord decompression usually can predict the impending neuromonitoring changes during spinal canal stenosis decompression.
- While patient going for neuronal decompressive surgery, during surgical procedure Motor evoked potential may alert a signal changes in moderate to severe spinal compressive myelopathy as a true positive or false positive its depend on types of signal .
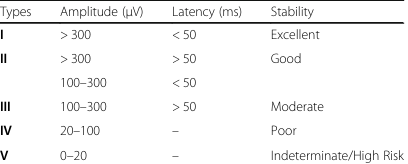
Different type of MEP baseline.
- Type I indicated safe MEP baseline with excellent stability.
- Type II also indicated safe MEP baseline with good stability.
- Type III was referred to sensitive MEP baseline with average stability.
- Type IV was high sensitive MEP with poor stability.
- Type V was indeterminate/high risk MEP baseline.
Here is details of different types of MEP baseline in microvolt.
Waveform of signals as per cervical cord compression.
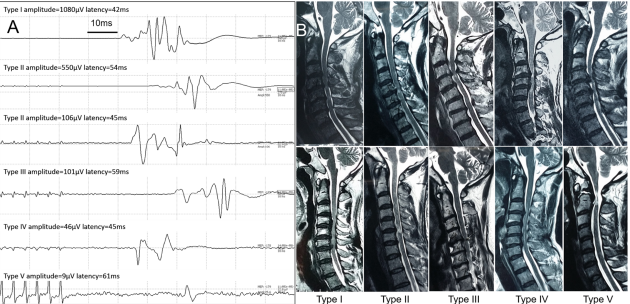
A The representative MEP waveform among the 5 baseline types. B The preoperative T2-weighted sagittal magnetic resonance image (MRI) from the patients with different MEP baseline types [Types I, II, III, IV and V)]
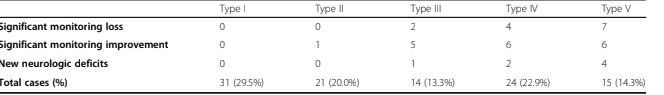
As per this journal [ Data analysis]
- No significant neuromonitoring change and postoperative new spinal deficit was found in Type I & II in 14 patients until unless any mechanical injury or reperfusion injury.
- Type III, 2 showed significant MEP losses 5 showed intraoperative MEP improvements.
- Type IV, 4 showed significant MEP loss, 6 showed MEP improvements.
- V, 7 showed significant MEP loss, 6 showed MEP improvements
- Reduction in MEP amplitude can predict decreased excitability or damage to the corticospinal tract. Monitoring changes in MEP amplitude provides insights into the functional status of the spinal cord
- Alterations in MEP waveform morphology, such as polyphasic to monophasic may indicate changes in cervical cord or motor system dysfunction in cord compression patients.
- During the procedure with the type I or II MEP baseline if shows drop the injuries degree of nervous tissue from blood supply or direct mechanical cord compression are probably in relative compensatory stage.
- On the other hand, that reperfusion lesions can result in neuronal death, which reactive oxygen radicals have been implicated to play an important role after decompression of a chronic compressive lesion of the cervical cord
Postoperative new spinal deficits.

The type I and II are safe and stable MEP baseline that generally does not present significant intraoperative monitoring changes until unless mechanical , traction or reperfusion injury. Type III and IV are sensitive MEP baseline little manipulation at cord during decompressing tight canal stenosis may change signal either true positive and false positive here as a clinician we have to understand if cord pulsating well and no other physiological changes, possibility of false drop of signal. type V is high risk MEP baseline that would imply a possibility of great neuromonitoring changes.

- [If you find any mistake or incomplete information In my medical article about intraoperative neurophysiological monitoring subject please do comment so that i can improve further.]
Related this article.
https://neurointraoperative.com/wp-admin/post.php?post=1849&action=edit
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10380862
Question.
How much amplitude of signals are important to interpret?
Why we need more than 300 microvolt MEP signals?.
What is the meaning of false positive?
Can we use another TIVA drugs to maintain baseline MEP?

3 thoughts on “Motor Evoked potentials in Cervical Cord Surgery when signal drops”